Parkinson’s disease is the second most common neurodegenerative disease. It leads to symptoms like trembling, stiffness and general slowness of movements. Over time, a person with Parkinson’s may have trouble talking, swallowing or sleeping. It affects around 1000 people in Luxembourg, and 7 to 10 million worldwide. In all likelihood, these numbers will double until 2050. Both genetic as well as environmental factors are thought to play a pivotal role in the faster ageing and degeneration of dopamine-producing nerve cells that underlie this disease. But how exactly they trigger the pathological process in those cells is not clearly understood yet.
At the LCSB, Parkinson’s disease is at the core of our research. Using the combined expertise of the centre, we look at it from all angles to understand the molecular mechanisms behind this disease: Can we define subgroups of patients based on molecular and clinical characteristics? What is the role of mitochondria, the powerhouses of the cells, in Parkinson’s disease? Can we find new biomarkers in blood or urine with which we could diagnose the disease earlier, before motor symptoms occur? Can personalised 3D nerve cell cultures derived from patients’ skins cells help to find new therapeutics? How can we improve existing care options for people with Parkinson’s disease? Can we predict how the disease will evolve over time for each patient? What is the role of the gut microbiome or of environmental factors in the development of the disease?
Diseases like Parkinson’s, Alzheimer’s and other neurodegenerative diseases do not develop overnight. The body changes slowly, unnoticed, unwatched until – suddenly – the symptoms arise. This process can sometimes take years. We research the causes of this slow development and the ultimate transition to find effective therapeutic approaches. Only then will we be able to progress from treating the symptoms to finally curing these diseases at their cause.
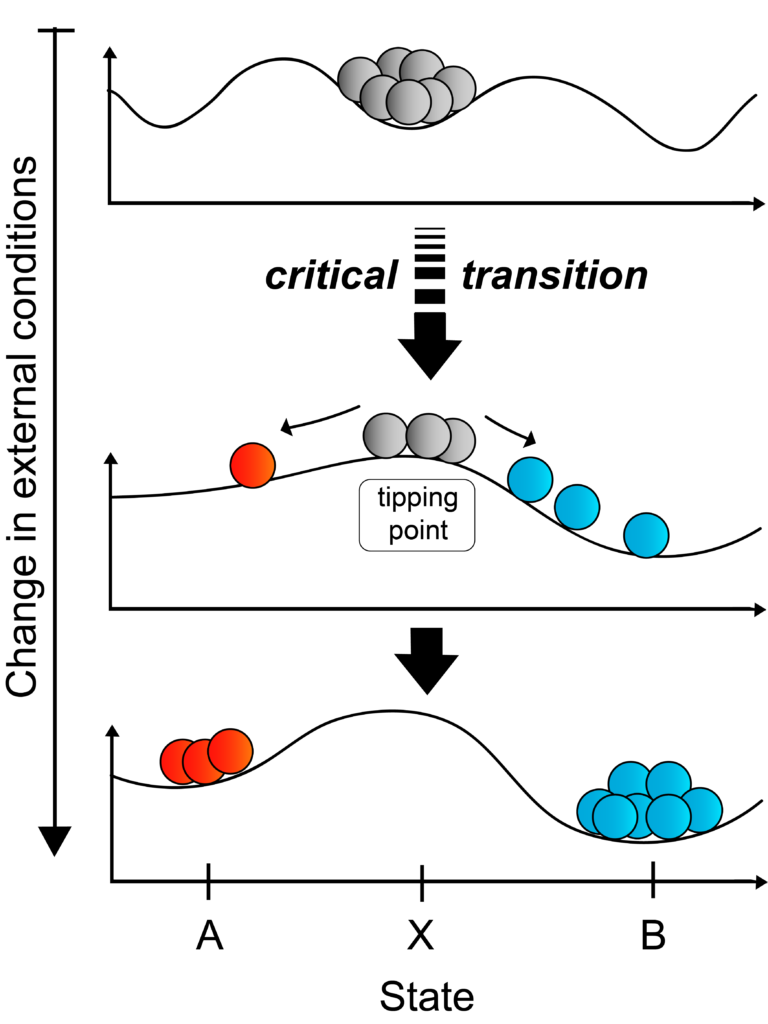
In science, such processes are called critical transitions. Whether at the onset of an epileptic seizure, a heart attack or a stock market crash, researchers can observe similar patterns at the start of such catastrophic shifts. The level of organisation inside a system increases significantly at first and then drops at a critical moment. At the LCSB, we study common mechanisms and shared properties between the different complex systems. We have dedicated one of our Doctoral Training Units to the topic of critical transitions, combining experimental and computational approaches. The aim is to predict when a disease will start and to determine early warning signals to prevent it.
Parkinson’s disease is the second most common neurodegenerative disease. It leads to symptoms like trembling, stiffness and general slowness of movements. Over time, a person with Parkinson’s may have trouble talking, swallowing or sleeping. It affects around 1000 people in Luxembourg, and 7 to 10 million worldwide. In all likelihood, these numbers will double until 2050. Both genetic as well as environmental factors are thought to play a pivotal role in the faster ageing and degeneration of dopamine-producing nerve cells that underlie this disease. But how exactly they trigger the pathological process in those cells is not clearly understood yet.

In 2015, the Luxembourg National Research Fund (FNR) established the National Centre for Excellence in Research on Parkinson’s disease, in which five research institutes in Luxembourg combine their expertise on Parkinson’s disease. The LCSB plays a key role in this collaborative research program, led by Prof. Rejko Krüger. More than 1400 volunteers with and without Parkinson’s have participated already in the Luxembourg Parkinson’s Study to find new ways to earlier diagnose and better treat the disease. Combining clinical and psychological information, as well as molecular data from biological samples like blood or urine, LCSB researchers are looking for new biomarkers that differentiate patients from people without Parkinson’s disease.
We aim to improve the therapy patients already receive today. In 2017, the LCSB has established ParkinsonNet Luxembourg, based on an integrated care concept developed in the Netherlands. ParkinsonNet trains healthcare professionals, e.g. physiotherapist, speech therapist and ergotherapist, for the treatment of Parkinson’s patients, following on evidence-based international guidelines, and facilitates the information exchange between the different healthcare disciplines. This puts the needs of the patients at the center and simplifies their access to specialised care

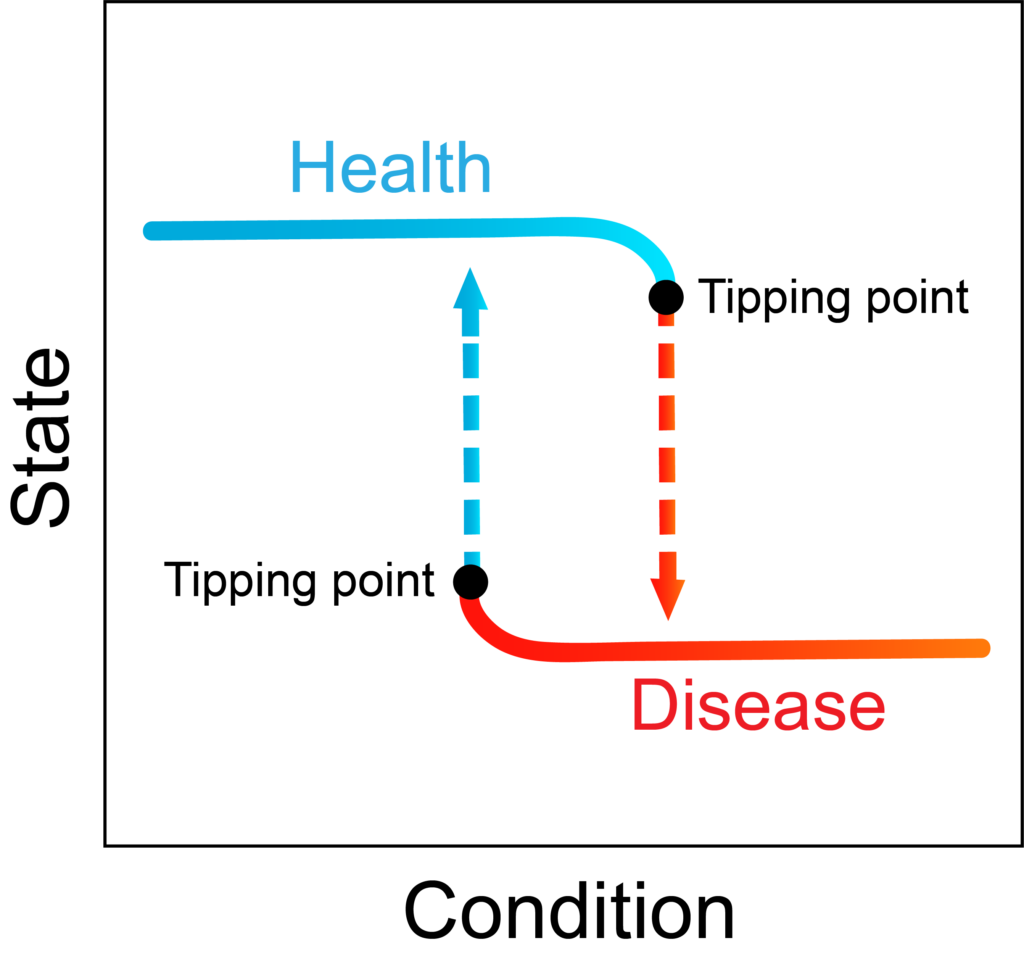
During the course of neurodegenerative diseases the body often changes slowly and unnoticed, until – suddenly – the symptoms arise. This catastrophic shift is preceded by a significant increased level of organisation inside a system at first and then a drop at a critical moment. At the LCSB, we study common mechanisms and shared properties between the different complex systems. By combining experimental and computational approaches we want to predict when a disease will start and to determine early warning signals to prevent it.
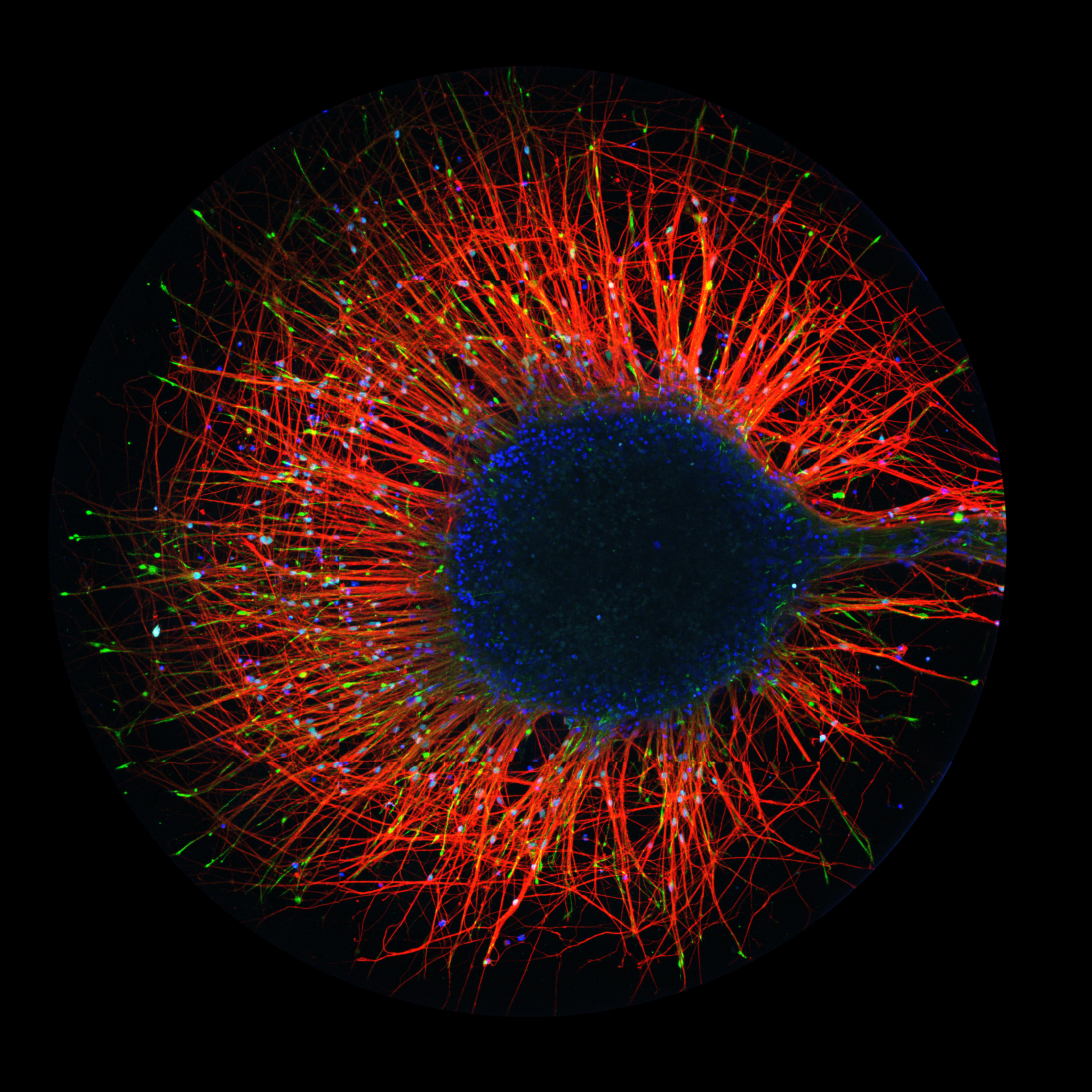
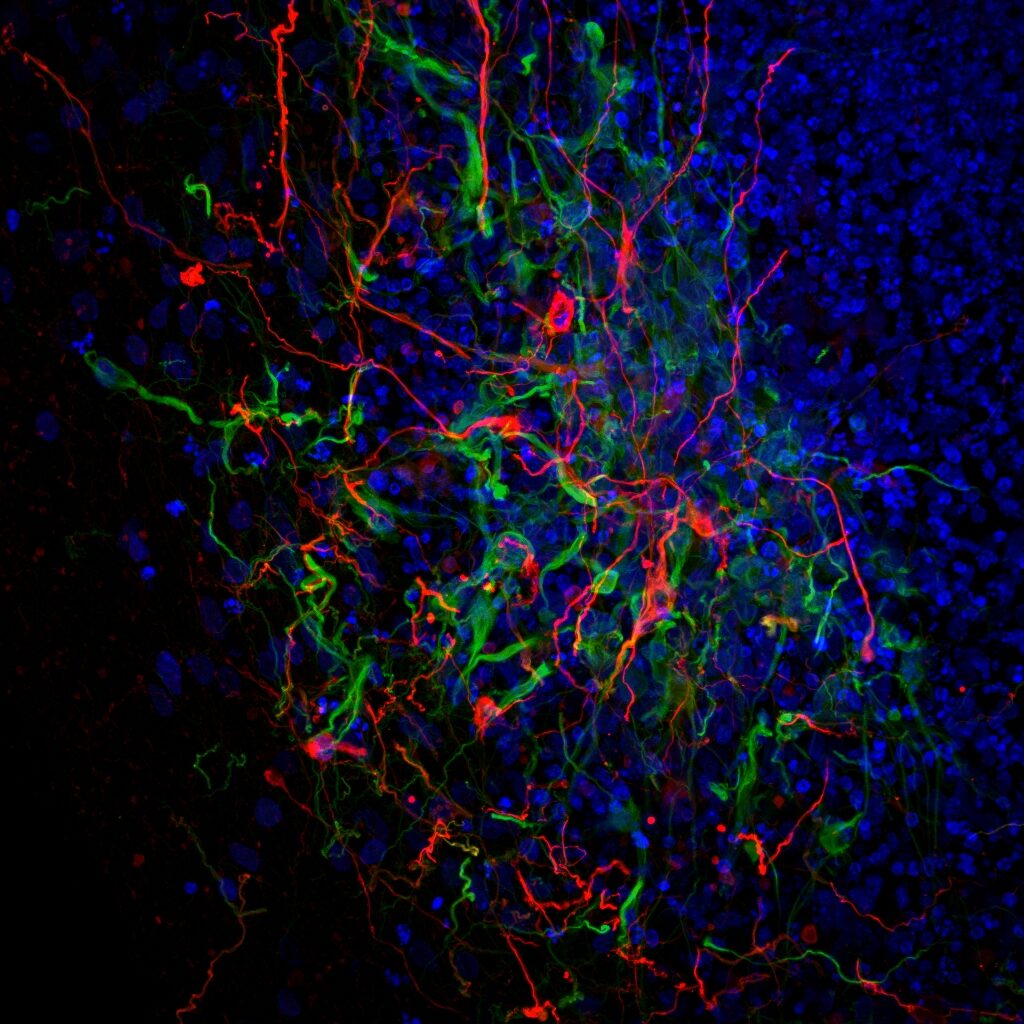
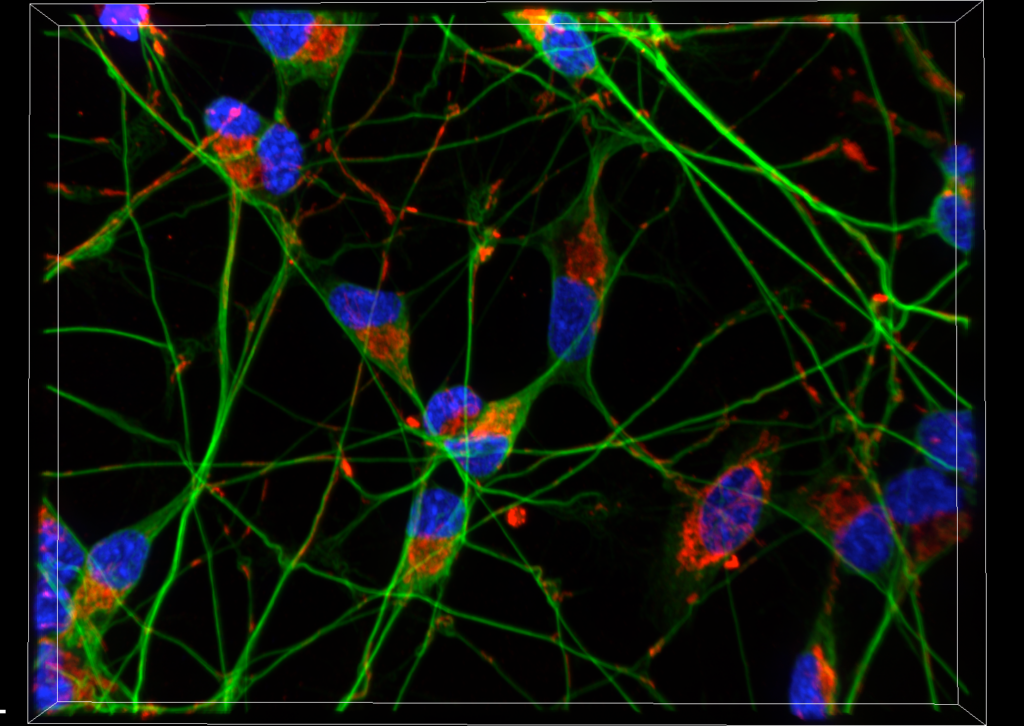
Parkinson’s disease is characterised by the specific degeneration of dopaminergic neurons and the presence of cytoplasmic inclusion bodies containing misfolded aggregated α-synuclein (α-syn) in the dopaminergic neurons that remain. We will investigate the interaction of pathogenic α-syn using cell lines with a patient genetic background. Drug screens of patient-specific dopaminergic neurons are used to determine the disease-modifying agents that are triggered by the action of pathogenic α-syn.
This LEIR-FNR INTER research project will be jointly conducted by the LCSB and the research group of Professor Serge Przedborski from Columbia University. This bilateral research project benefits from the expertise of the Przedborski lab and the unique α-syn patient-based cellular models and high-content high-throughput compound screening expertise available at the Krüger lab.
© 2026 LCSB Fundraising
Legal notices
Design by Marc Wilmes Design
